Age - Related Macular Degeneration (AMD) In The Elderly
Among other degenerative conditions, vision impairment is one of the leading causes of morbidity in the elderly. Since people get older, there are greater risks to develop age-associated eye diseases and conditions that potentially lead to vision loss. One of eye problems frequently found in elderly people is age-related macular degeneration, known shortly as AMD. To prevent vision loss, awareness and regular eye screening are vital. If abnormalities are early detected and diagnosed, timely and appropriate treatments can be given accordingly, resulting in decreased severity and delayed disease progression.
Get To Know Age – Related Macular Degeneration (AMD)
Age-related macular degeneration happens when the macular which is the central area of the retina responsible for clear vision in the direct line of sight begins to deteriorate. If age-related macular degeneration develops without proper and timely treatments, it eventually causes central vision loss. Age-related macular degeneration is characterized by drusen, defined as small yellow deposits of fatty proteins or lipids that accumulate under the retina, the alterations of retinal pigment epithelium (RPE) and the formation of choroidal neovascular membranes which are new blood vessels. Vision loss can be caused by this abnormal blood vessel growth. Sometimes abnormal new blood vessels grow from the choroid under and into the macula (known as choroidal neovascularization). The choroid is the layer of blood vessels between the retina and the outer, firm coat of the eye (sclera). These abnormal blood vessels may leak fluid or blood (subretinal fluid), interfering with the retina’s function and causing subretinal hemorrhage, an accumulation of blood between the neurosensory retina and RPE. In addition, subretinal fibrosis, defined as the development of band- or plaque-like areas of fibrosis underneath the retina can also be formed.
Types Of AMD
There are two types of age-related macular degeneration:
- Dry AMD: A number of drusen, small yellow deposits of fatty proteins or lipids that accumulate under the retina are typically found in dry macular degeneration. Geographic atrophy, a late-stage of dry age-related macular degeneration might develop. Dry AMD is more common, accounting for 85-90% of all cases. It usually progresses slowly and rarely causes total blindness.
- Wet AMD: Although wet AMD only accounts only for 10-15% of patients with AMD, this type is more likely to cause a relatively sudden change in vision, resulting in serious vision loss due to the formation of new blood vessels that grow from the choroid under and into the macula (choroidal neovascularization). As a result, it causes subretinal hemorrhage, fluid leakage and subretinal fibrosis underneath the retina, leading to total vision loss.
Risk Factors Of AMD
The exact cause of the deterioration remains unknown, but other risk factors play a major role in development of AMD. These include:
- Advanced age: People aged over 75 are at 3 times greater risk of having AMD than people aged 65-74.
- Smoking: Smoking cigarettes significantly increases the risk of macular degeneration. Smokers are at 2 times greater risk of vision loss caused by AMD, compared to non smoking ones. Former smokers who have stopped smoking, risk of vision loss slightly increases with odd ratio 1.13. However, if smoking cessation lasts longer than 20 years, risks to develop vision loss due to AMD in former smokers are equivalent to non smoking groups.
- Genetics: This disease has a hereditary component since a number of researches have identified several genes that are related to developing the condition and responding to the treatments. This might be beneficial to treatment options in the future.
- Other contributing factors: Other conditions that might increase risk of AMD are:
- Cardiovascular disease;
- Hypertension;
- Being female;
- Being white people;
- High blood cholesterol;
- Obesity;
- Farsightedness (hyperopia);
- Family history and
- Having light iris color.
Signs And Symptoms Of AMD
Warning signs and symptoms of age-related macular degeneration include:
- Worsening or impaired vision. If only one eye is affected, patient might not notice any changes in vision since good eye may compensate for an affected eye. Vision impairment can gradually or suddenly happen;
- Blurred vision;
- Distorted vision with fuzzy or wavy images and
- Dark spots in the central area of an object with reduced central vision.
Diagnosis Of AMD
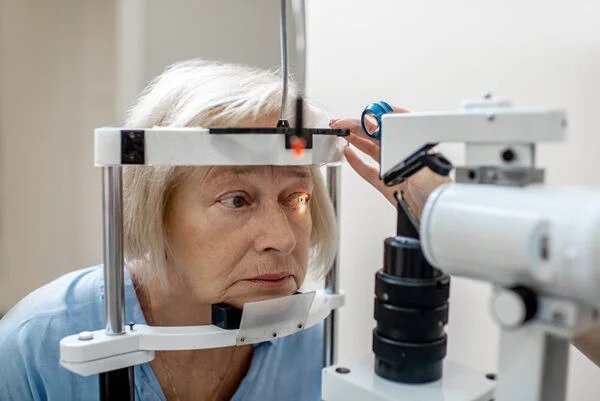
Early detection and treatment of AMD can substantially help reducing vision loss and perhaps recovering vision in some instances. To confirm a diagnosis of AMD, several tests conducted by an ophthalmologist include:
- Visual acuity which is the eye exam to measure the clearness or sharpness of vision.
- The slit lamp exam, or also known as biomicroscopy that combines a microscope with a very bright light in order to look for eye injuries or diseases.
- Using pupil dilation medications in form of eye drops to investigate eye abnormalities such as a mottled appearance caused by drusen. Sunglasses should be worn after the test and self-driving is not recommended since medications dilate pupils, causing side effects, such as blurred vision and light sensitivity which normally last for 4-6 hours.
- Fundus photography
- Optical coherence tomography or OCT. OCT is non-invasive imaging test which displays detailed cross-sectional images of the retina. It identifies the area of retinal thinning, thickening or swelling which can be caused by fluid accumulations from leaking blood vessels in and under the retina.
- In case that wet AMD is suspected, fundus fluorescein and indocyanine green angiography (FFA and ICGA) are needed for differential diagnosis in order to receive appropriate treatments accordingly.
Treatment Of AMD In The Elderly
If age-related macular degeneration is indicated, treatments provided by expert ophthalmologists must be initiated as soon as possible in order to slow disease progression and reduce risks of vision loss. However, there are currently no documented cures for age-related macular degeneration. Recommendations include:
- Prevention: Avoid risk factors e.g. smoke cessation, maintaining healthy weight and keeping blood pressure under control.
- Treatment of dry AMD: To treat dry AMD, antioxidants and mineral supplements can help delay disease progression. Based on the results of clinical trials, AREDS and AREDS2, certain antioxidants and supplements reduce the risks to develop geographic atrophy which is an advanced stage of disease up to 25% and they can also lower the risks of central vision loss 19%.
- Treatment of wet AMD: Currently, the most effective treatment is certain medications that help inhibit the growth of new blood vessels by blocking the effects of growth signals that the body sends to generate new blood vessels. These drugs are widely used and considered the first line treatment for all stages of wet macular degeneration. Administered via ocular injection, two groups of these medicines are:
- Anti–Vascular Endothelial Growth Factor or anti-VEGF e.g. Bevacizumab and Ranibizumab
- Vascular Endothelial Growth Factor Trap or VEGF-Trap e.g. Aflibercept
- Other treatment option for wet AMD: Other options might include photodynamic therapy and laser photocoagulation. Photodynamic therapy uses certain drug to stop the leakage of blood vessel, resulting in improved vision and reduced the rate of vision loss. While laser photocoagulation uses a high-energy laser beam to seal abnormal blood vessels under the macula. However, select treatments are determined by expert ophthalmologists which might vary among individual patients, depending primarily on patient’s conditions and disease