Meibomian Gland Dysfunction (MGD), One Of Contributing Factors To Dry Eye Syndrome
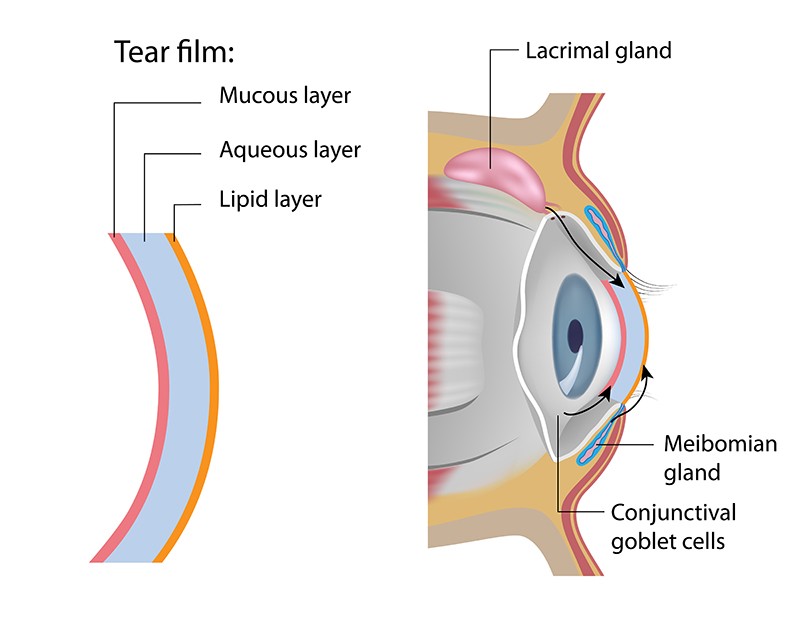
Experiencing symptoms e.g. eye irritation, redness, discharge, easily fatigued eyes and blurred vision might be potentially associated with dry eye syndrome. One of contributing factors to dry eye syndrome is meibomian gland dysfunction (MGD) defined as blockage or other abnormality of the meibomian glands, tiny oil glands which line the margin of the eyelids. The normal tears are made up of three layers – a lipid layer, a watery or aqueous layer and a mucous layer. If the oil gland openings get plugged up or obstructed, meibomian glands do not secrete sufficient oil into the tears, leading to evaporative dry eye that often causes eye irritation and eye lid infections. Knowing warning signs of meibomian gland dysfunction allows for early diagnosis and appropriate treatments before dry eye syndrome develops.
Get To Know Meibomian Glands
Meibomian glands are the tiny oil glands which line the margin of the eyelids. There are approximately 30 to 40 meibomian glands in the upper eyelid and 20 to 30 glands in the lower eyelid. These glands secrete oil which coats the surface of the eyes and keeps the water component of tears from evaporating. Tear film is made up of three intertwined layers – a lipid layer, an aqueous layer and a mucous layer. These three layers work collaboratively to help maintain the health of the eyes and prevent eye infection. Particularly, the lipid layer is an essential component of the tear film, providing a smooth optical surface and retarding evaporation from the eye.
Meibomian Gland Dysfunction
The meibomian glands normally secrete a lipid secretion, known as meibum which is a clear or pale yellow oily liquid. Without any abnormality, this oily liquid is easily secreted from the meibomian glands. However, if meibomian glands do not function properly, lipid secretion turns to be more cloudy and sticky, leading to the obstruction of the gland openings located on the edge of eyelids. Meibomain gland obstruction impedes lipid secretion into the tear film characterized by a low delivery state. As a result, tear film loses its stability and becomes evaporative easily, leading to eye irritation and dry eye. In addition, the plugged lipid can accumulate, presenting as the thickened lipid on the edge of eyelids, leading to an increased risk of bacterial infections and increased amount of eyelash mites (dermodex).
Meibomian gland dysfunction is characterized by blockage or other abnormality of the meibomian glands that results in impaired lipid secretion, leading to evaporative dry eye. Moreover, meibomian gland dysfunction is associated with other eye conditions e.g. blepharitis and stye –a bacterial infection of meibomian glands in the eyelid.
Risk Factors
Meibomian gland functions can be altered through several factors, including:
- Aging: Age over 40 is a known risk factor for meibomian gland dysfunctions. With age, meibomian gland exhibits decreased lipid production and altered meibum composition with changes in lipid profiles.
- Wearing eye makeup. The most likely cause is an eye makeup technique called inside liner. After wearing, if this makeup is not fully removed, it potentially induces the obstruction of meibomian glands.
- Contact lens. The use of contact lenses is associated with reduced meibomian gland morphology and function, causing eye irritation and altered blinking patterns.
- Computer or mobile screen. Computer eye strain can cause meibomian gland dysfunction due to a reduction in blinking that leads to less lipid secretion and eventually tear film instability.
- Other Eye diseases e.g. allergic conjunctivitis and other health issues e.g. hypertension and rheumatoid arthritis as well as side effects of certain medications, such as anti-acne and psychiatric medicines can induce meibomian gland dysfunction.
Diagnosis
Since manifestations of meibomian gland dysfunction — red eyes, a gritty feeling, itchy eyes and blurred vision are nearly the same as those of dry eye syndrome, a comprehensive eye examination and diagnosis must be thoroughly conducted by expert ophthalmologists. To perform basic screening test for meibomian gland dysfunction, an ophthalmologist may press on the eyelids to squeeze oil out and examine an altered quality and quantity of expressed oil secretions. Moreover, the amount and quality of tear film will be furthered analyzed in order to make a conclusion for definite diagnosis.
Treatments
- Lifestyle modification. In patients with mild symptoms, lifestyle modifications are highly advised . These include: taking eye breaks during long tasks e.g. taking a 20-second eye break every 20 minutes, looking at far distance 20 feet away and frequent blinking.
- Artificial eye drops. Artificial eye drops can be used as prescribed for moisturizing eyes and enhancing eye comfort.
- Lid hygiene. Lid hygiene is essential for good eye care since it plays a fundamental role in decreasing the viscosity of lipid layer and enhancing lipid secretion from meibomian glands, enabling the tear film to lubricate the ocular surface more efficiently. Applying lid hygiene substantially helps prevent tear film from evaporating, resulting in a significant reduction of risk to develop evaporative dry eye. A lid hygiene regimen include 3 steps: eyelid warming, eyelid massaging and eyelid cleansing.
- Eyelid warming. Warm compress acts as a mainstay of treatment to soften the meibum that obstructs the meibomian glands, enabling it to flow out of the meibomian glands more easily. To apply warm compress, warming devices can be heated gel pack, warm washcloth and medical devices such as the Blephasteam® – an eyelid-warming device which constantly provides gentle heat to the eyelids. The optimal temperature should be set at 40 degrees Celsius and the constant compress should be gently applied to both eyelids for 10 – 15 minutes. If heated gel pack or washcloth is used, an optimal temperature should be ensured, neither too hot nor too cold. A clean, moistened washcloth can be reheated for a constant temperature applied to the eyelids.
- Eyelid massaging. The goal is to express any thickened oil clogging the openings of meibomian glands. To massage the eyelids, use the index finger or middle finger and sweep the pad of that finger from the inner corner of the eye along the eyelid to the outer corner of the eye. While massaging the upper eyelid, look down and vice versa. Massaging should neither to be too gentle nor too firm.
Eyelid cleansing. Eyelid cleansing can be performed simply by using cotton tips or pads wetted in the cleansing solutions made of clean water and baby shampoo at a ratio of 1:10. In some cases, an ophthalmologist might prescribe eyelid cleanser solutions for cleaning the edge of eyelids and the base of eyelashes once or twice a day after a warm compress.

After using artificial tear drops regularly combined with lid hygiene, if the symptoms do not subside, it is highly recommended to further seek medical assistance. Additional treatments often involve:
- Using azithromycin ophthalmic solution or ointment for eradicating bacteria that cause eyelid infection and inflammation.
- Taking oral doxycycline for adjusting lipid component and decreasing inflammation of the meibomian glands in addition to its antibiotic properties against bacterial infections.
- Taking foods or supplements that are high in omega-3, such as cold-water fatty fish or flaxseed oil. Regarding certain medical studies, omega-3 fatty acid has been recommended to help improving dry eye caused by meibomian gland dysfunction.
- Using cyclosporine and/or steroid eye drops. These medications are only prescribed in patients who develop severe corneal and eyelid inflammations. Due to certain side effects, especially an elevated intraocular pressure and increased risk of glaucoma, steroid eye drops can be used only for a short period of time under close supervision of the specialists.
Disease Severity
If meibomian gland dysfunction is left untreated, the condition might severely progress. Over time, the glands become completely obstructed, which then leads to meibomian gland atrophy, resulting in permanent changes in the tear film and dry eyes. Serious complications in patients with late stage often include eye irritation, eyelid pain and chronic evaporative dry eye that significantly increases the risk of eye infections although some patients might not exhibit any symptom in earlier stages.
If meibomian gland dysfunction is diagnosed, appropriate treatments should be provided in a timely manner. All prescribed medications and self-instructions must be strictly taken, including eyelid warming, massaging and cleansing. In addition, risk factors that profoundly aggravate symptoms must be avoided.